
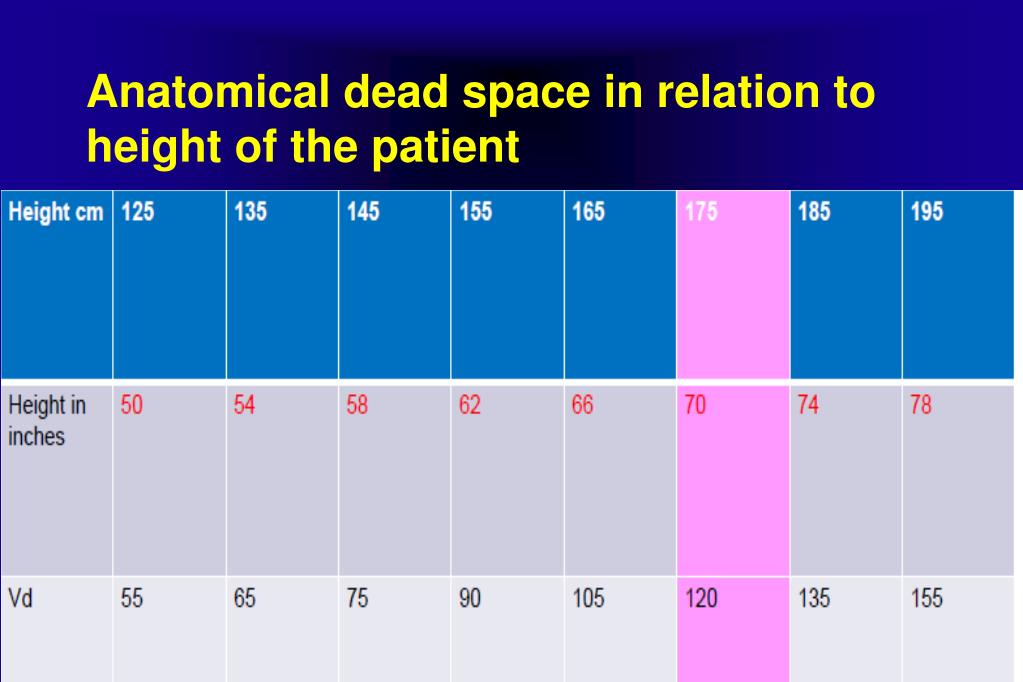
Understanding each piece separately and their role will allow for optimal treatment and improved results.\): Chronic Obstructive Pulmonary Disorder. The role of FiO2 in normoxemic and hypoxemic patients has yet to be determined.Īnatomical dead space is just a piece in physiological dead space. Assessment of minute ventilation is a better predictor in the reduction of anatomical dead space with high flow therapy than FiO2. Adjusting flows to meet the inspiratory demands of the patient and reducing the work of breathing will reduce the rebreathing and improve wash out, thus, decreasing the dead space. A reduction in respiratory rate has shown to correlate to a reduction in dead space and improved alveolar ventilation. Selection of proper flow will reduce the respiratory rate. Flow (dose) affects the time (respiratory rate).

Clearance of expired air causes a reduction in dead space, but it is dose and time dependent. Understanding the importance of dead space and its indication of overall lung function will prove beneficial to patient outcomes.Īssessing the dead space throughout ventilation and treating with high flows is a key mechanism for decreased anatomical dead space.
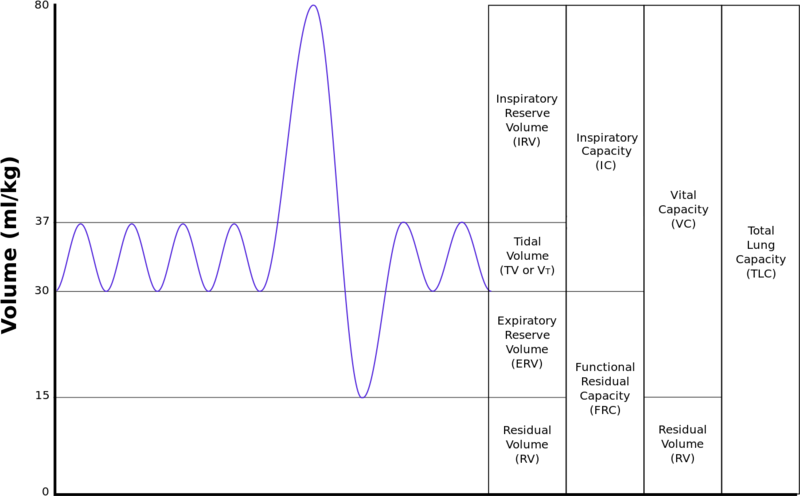
Anatomical dead space is only part of physiological dead space. Dead space is an intrinsic part of volume capnography and a significant value for clinical situations.


 0 kommentar(er)
0 kommentar(er)
